Contact us
- Understanding Bone Marrow and Stem Cells
- What is a Bone Marrow Transplant?
- Types of Bone Marrow Transplant
- Why is a Bone Marrow Transplant Needed?
- How the Bone Marrow Transplant Process Works?
- Recovery and Life After BMT
- Possible Risks and Complications
- Global Perspective: BMT Success and Evolution
- Bone Marrow Transplant Cost in India
- Why Choose India for a Bone Marrow Transplant?
- Top Hospitals for Bone Marrow Transplant in India
- Renowned BMT Specialists in India
- Life After BMT: Tips for Long-Term Health
- The Emotional Journey: Beyond Medicine
- Conclusion
Imagine being told your body can no longer make healthy blood, the very essence that keeps you alive. For patients with severe blood cancers, genetic disorders, or bone marrow failure, this can feel like an ending.
But thanks to medical science, it’s often the beginning of a new chapter.
A Bone Marrow Transplant (BMT), also known as a Stem Cell Transplant, gives thousands of people worldwide a second chance at life. It replaces damaged or diseased bone marrow with healthy stem cells, restoring the body’s ability to produce blood and rebuild immunity.
In this blog, we’ll explore what a bone marrow transplant is, how it works, who needs it, what recovery looks like, and yes, what it costs, especially in India, where it’s become one of the most accessible and advanced treatments globally.
If you or someone you love is facing a BMT, take a deep breath. Help, hope, and healing are possible.
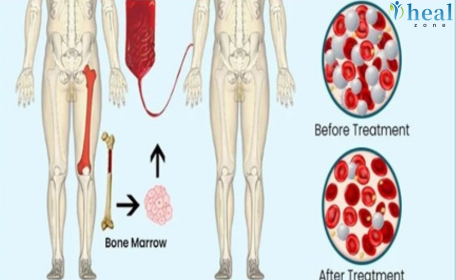
Understanding Bone Marrow and Stem Cells
Bone marrow is a soft, spongy tissue that is found inside your large bones, like your hip and thigh bones. It’s home to hematopoietic stem cells, which are immature cells that develop into:
- Red blood cells (RBCs) carry oxygen.
- White blood cells (WBCs) fight infection.
- Platelets help clot blood and stop bleeding.
When the bone marrow fails due to cancer, disease, or certain treatments, the body cannot make enough healthy blood cells. That’s when doctors recommend a Bone Marrow Transplant to replace the faulty marrow with healthy stem cells that can rebuild the system.
What is a Bone Marrow Transplant?
A Bone Marrow Transplant (BMT) is a procedure where damaged or destroyed bone marrow is replaced with healthy stem cells. These stem cells may come from the patient’s own body or from a donor.
Contrary to what many believe, BMT is not an open surgery. Healthy stem cells are infused into the patient's bloodstream through an IV line, much like a blood transfusion. Once infused, the new cells travel to the bone marrow spaces, settle there, and start making healthy new blood cells.
Types of Bone Marrow Transplant
Bone marrow transplants are classified based on where the stem cells come from.
1. Autologous Transplant
- The patient’s own stem cells are collected before high-dose chemotherapy or radiation and infused back afterward.
- Common in multiple myeloma and lymphoma.
- Lower risk of rejection or complications.
2. Allogeneic Transplant
- Stem cells come from a donor, usually a sibling, parent, or unrelated match.
- Used for leukemia, aplastic anemia, and genetic blood disorders.
- Requires immunosuppressive drugs to prevent graft rejection.
3. Haplo-Identical Transplant
- Uses a half-matched donor (parent or child).
- Expands donor options when a full match isn’t available.
4. Cord Blood Transplant
- Uses stem cells from umbilical cord blood, often for children or smaller adults.
- Each transplant type comes with its own preparation, benefits, and challenges. The choice depends on disease type, patient age, donor availability, and medical condition.
Why is a Bone Marrow Transplant Needed?
A BMT becomes necessary when a patient’s bone marrow stops functioning properly or produces abnormal blood cells.
It’s often the only curative treatment for many life-threatening conditions.
Common Conditions Treated by BMT:
- Leukemia (Blood Cancer) – Abnormal white cells crowd out healthy blood.
- Lymphoma – Cancers of the lymphatic system that may spread to the marrow.
- Aplastic Anemia – Marrow stops producing blood cells entirely.
- Thalassemia & Sickle Cell Anemia – Inherited disorders causing abnormal hemoglobin.
- Multiple Myeloma – A cancer of plasma cells.
- Severe Immune Deficiencies – Where the immune system fails to protect the body.
In many of these conditions, BMT offers the only chance for long-term remission or cure.
How the Bone Marrow Transplant Process Works?
A bone marrow transplant involves multiple stages spread over weeks or months. Here’s what the journey typically looks like:
Pre-Transplant Evaluation
- Physical examination and fitness assessment
- Blood tests, imaging, and bone marrow biopsy
- Identification and HLA typing of potential donors
- Infection screening (HIV, Hepatitis, CMV, etc.)
Conditioning or Preparative Regimen
- Prior to the transplant, patients undergo intensive chemotherapy and/or radiation to eliminate abnormal cells and weaken the immune system, making room for healthy stem cells to engraft.
Stem Cell Collection
- For an autologous transplant, the patient’s own stem cells are collected through a process called apheresis.
- For an allogeneic transplant, stem cells are collected from the donor’s blood or bone marrow.
Transplant Day (“Day 0”)
- Healthy stem cells are then infused into the patient’s bloodstream. This process takes 1 to 3 hours and is completely painless.
Engraftment
- Within 10 to 25 days, the new cells start producing healthy blood. Doctors closely monitor this phase for infections, fever, and graft reactions.
Post-Transplant Recovery
- The patient stays in a HEPA-filtered isolation room for 3–6 weeks.
- Regular monitoring of blood counts, electrolytes, and liver function.
- Gradual tapering of medications as immunity recovers.
- This phase requires patience, but each day marks progress toward recovery and independence.
Recovery and Life After BMT
Recovery doesn’t end at discharge; it continues for months as the new immune system develops.
Early Recovery (First 3 Months)
- Regular hospital visits for monitoring
- Strict hygiene and infection control
- Controlled diet: no raw foods, only cooked meals
- Protective masks and minimal crowd exposure
Intermediate Phase (3–6 Months)
- Energy levels improve
- Hair and appetite return
- Mild fatigue may persist
- Immunity gradually strengthens
Long-Term Recovery (6–12 Months)
- Return to normal work or school
- Gradual reduction in medications
- Periodic checkups and vaccinations resume
- Patients describe this phase as a rebirth, a return to normalcy after months of struggle. With discipline and care, most people go on to live full, healthy lives.
Possible Risks and Complications
Like any major medical procedure, a BMT carries some risks. However, modern protocols and advanced monitoring have drastically improved outcomes.
Short-Term Risks
- Fever or infections
- Nausea, fatigue, and mouth sores
- Temporary hair loss or appetite loss
Long-Term Risks
- Graft-versus-Host Disease (GVHD), when donor cells attack host tissues
- Organ toxicity from chemotherapy
- Fertility issues (discussed before treatment)
Doctors manage these risks with preventive antibiotics, immunosuppressants, and regular monitoring. The good news? Most complications are manageable and temporary.
Global Perspective: BMT Success and Evolution
Bone marrow transplantation has evolved tremendously over the last two decades. Today, more than 80,000 transplants are performed worldwide each year, with rising survival rates even in advanced diseases. In countries like India, Singapore, and Turkey, the availability of world-class infrastructure and skilled specialists has made BMT both affordable and accessible to international patients.
Bone Marrow Transplant Cost in India
While this blog focuses on the medical and human side of BMT, it’s natural to wonder about costs, especially if you’re planning treatment.
|
Type of Transplant |
Average Cost (USD) | Hospital Stay (Days) |
|
Autologous (Self) |
18,000 - 22,000 | 21 - 30 |
|
Allogeneic (Donor) |
20,000 - 25,000 | 30 - 45 |
|
Haplo-Identical / Half-Matched |
22,000 - 30,000 | 30 - 50 |
|
Matched Unrelated Donor (MUD) |
25,000 - 30,000 | 40 - 55 |
India offers one of the most cost-effective bone marrow transplant programs in the world, without compromising on quality or outcomes.
Why Choose India for a Bone Marrow Transplant?
India has rapidly emerged as one of the world’s most trusted destinations for bone marrow transplantation, offering a rare blend of affordability, advanced technology, and world-class expertise. The overall cost of a BMT in India is 3–4 times lower than in the US, UK, or Europe, and that too without compromising on quality or outcomes. This cost advantage allows patients to receive cutting-edge treatment at just a fraction of international prices.
Indian hospitals are internationally accredited by organizations such as NABH and JCI, ensuring strict global standards in hygiene, safety, and patient care. These centers are equipped with HEPA-filtered isolation rooms, advanced stem cell labs, and 24×7 infection control systems—matching the best in the world.
Equally impressive is India’s pool of globally trained hematologists and transplant specialists who handle thousands of successful transplants each year, including complex pediatric and haplo-identical cases. Additionally, shorter waiting times mean patients can start treatment almost immediately, crucial for life-threatening diseases where every day counts.
When compared with other medical destinations, India offers unmatched value, combining medical excellence, compassionate care, and personalized attention, making it a true global leader in affordable, high-quality bone marrow transplantation.
Top Hospitals for Bone Marrow Transplant in India
Some of the top Indian hospitals well known for BMT are:
- Apollo Hospitals (Delhi, Chennai, Hyderabad)
- Fortis Memorial Research Institute, Gurgaon
- Medanta – The Medicity, Gurgaon
- Tata Memorial Hospital, Mumbai
- BLK-Max Super Specialty Hospital, Delhi
- Global Hospitals, Hyderabad
- Amrita Hospital, Faridabad
These hospitals are pioneers in hematology and transplant medicine, equipped with advanced HEPA isolation wards and round-the-clock infection control.
Renowned BMT Specialists in India
Some of the top BMT specialists in India are:
These experts have performed hundreds of successful transplants with high survival rates and international acclaim.
Life After BMT: Tips for Long-Term Health
Life after a transplant can be remarkably fulfilling, but it requires care and vigilance. For several months, patients must avoid infections, eat carefully prepared food, and take medications to support immune function. Vaccinations are reintroduced gradually once the immune system stabilizes.
Physically, most people regain normal strength within a year. Emotionally, it may take longer to fully adjust. Many patients describe the first year after BMT as a time of rediscovery, learning to trust their body again, re-engaging with life, and finding purpose beyond illness.
Doctors often remind patients that every day post-transplant is a milestone. Every step, from the first normal blood count to the first day back at work, is a victory worth celebrating.
The Emotional Journey: Beyond Medicine
A bone marrow transplant is as much an emotional journey as a medical one. It challenges not only the patient’s body but also their spirit. The weeks in isolation, the uncertainty, and the slow path to recovery can test anyone’s strength. Yet, within these challenges lie stories of extraordinary resilience. Parents donate their cells to save their children. Siblings become each other’s lifelines. Entire families rally around one person’s fight.
Doctors often call BMT “a treatment of teamwork” because success depends not just on medicine, but on love, discipline, and support. Patients who maintain a positive outlook and have strong family involvement often recover faster and more completely.
Conclusion
A bone marrow transplant is one of modern medicine’s most powerful symbols of healing. It transforms despair into hope, not just medically, but emotionally and spiritually. India has become a global leader in bone marrow transplantation, offering world-class care at accessible costs. With the right team, proper guidance, and support from healthcare partners like HealZone, patients can embark on this journey confidently. A transplant doesn’t just change blood, it changes lives. Because sometimes, starting over is the bravest thing the body can do.
Contact us
Written by
B.Sc. & M.Sc. in Medical Imaging Technology
Frequently Asked Questions
The transplant itself is painless; it’s like receiving a blood transfusion.
Most patients recover in 3 to 6 months, with gradual improvement in energy and immunity.
Yes. In haplo-identical transplants, parents or children can donate stem cells.
Risks exist, but with modern facilities and close monitoring, success rates are high.
Around 70-90%, depending on disease type, donor match, and hospital expertise.
Doctors use HLA (Human Leukocyte Antigen) testing to match genetic markers between the patient and potential donors. If a family match isn’t available, registries like DATRI or WMDA are used to locate unrelated donors worldwide.
Yes, children can safely undergo bone marrow transplants, especially for conditions like thalassemia or leukemia. Pediatric transplant centers have excellent success rates, and most children recover faster than adults with proper post-care.
In a bone marrow transplant, stem cells are collected directly from the bone marrow, while in a stem cell transplant, they’re collected from the bloodstream through a process called apheresis. Both aim to restore healthy blood cell production.
Most patients stay in the hospital for 3–6 weeks, depending on their recovery and transplant type. International patients often remain in India for an additional few weeks for post-transplant follow-up and stability checks.
Patients should maintain strict hygiene, eat cooked, nutritious food, and avoid crowded places during recovery. Gentle exercise, rest, and regular follow-ups help rebuild immunity and improve long-term outcomes.
Latest Blogs
Reviews
I am Fadel Abu Muhammad from Tal Afar, Iraq My father had a brain tumor. We traveled to India to Accord Specialty Hospital, New Delhi, through a resident professor, Muhammad, Dr. Vikram, who called for a laparoscopic tumor removal operation. Thank God I thank the translator, the doctor, and all the hospital staff.
Posted On
I am Muhammad Reda from Baghdad, Iraq I was suffering from weakness in my left hand. I underwent tests and it turned out that I had a brain tumor. The translator, Muqeem Muhammad, contacted us and we traveled to India. I had a neuronavigation procedure performed by Dr. Sandeep Vashya Praise be to God, the operation was completed successfully on the computer At Fortis Hospital New Delhi I thank the translator and the doctor
Posted On
All our gratitude and appreciation to the wonderful translator Mohammed Muqeem, who was truly a great support and companion during our journey for my mother’s treatment in India. He was extremely helpful, deeply understanding of all our needs, patient, and dedicated in his work, which eased a lot of the hardship and challenges we faced being away from home. His presence with us was not just about translating words but about offering real human support in every situation and every moment. May God bless him and reward him greatly for all he has done for us.
Posted On
I'm Emad Mohammed Khadir from Iraq. I was suffering from cirrhosis and liver cancer. I came to Fortis Hospital in India to see Dr. Ankur Bahil, a consultant oncologist, with the help of our translator, resident professor Mohammed Al Hindi. Thank God, we received our chemotherapy doses. The doctor and all the hospital staff were very kind and helpful. May God bless them all. Thank you.
Posted On
I am Redha Fadel from Nasiriyah, Iraq. I had a bone tumor, osteosarcoma. I traveled to India to see Dr. Ankur, a cancer specialist at Fortis Hospital, with the help of Hill Zone Medical Tourism Company, Professor Muqeem Muhammad Al Hindi. I thank you for your humanity and services.
Posted On
Peace be upon you. I am from Iraq. My brother is suffering from a tumor in his left thigh (osteosarcoma). We came to Al-Nahda for treatment. We stayed at Fortis Hospital for two months. We are now going to Iraq and will return to India to complete the treatment and the joint replacement surgery. I would like to thank the polite Indian translator, Muqeem Mohammed Al-Hindi. He was our brother before he was a translator and he helped us a lot with my brother's illness. Thank you, Muqeem. Thank you, Fortis Hospital. Thank you, Dr. Ankur.
Posted On
Peace be upon you, I'm from Iraq. My name is Majid Mazhar Kazim. My brother was suffering from tumors, so we contacted a resident professor, Muhammad Al-Hindi, and we sent him medical reports. He received us from the airport in New Delhi. I highly recommend him to Iraqi patients. He is helpful and well-mannered. He didn't hold back on us and didn't leave us alone from the first day until the last. He also took us to the airport. I thank them all.
Posted On
I am Mohammed Kazim from Iraq, from Babylon. My brother Mushtaq was suffering from meningitis. We came to India to Fortis Hospital through our resident professor, Mohammed, the director of Hill Zone Medical Services. I thank them for their kind treatment and translation. It was an enjoyable and fruitful trip. Praise be to God.
Posted On
I am from iraq tilafar, i came to India for my treatment an immune disease, i am thankful to Mr Muqeem and hospital staff, Marego Asia Hospital
Posted On
I am from Iraq. My son was suffering from Hirayama disease. I called Heal Zone, and they arranged our treatment journey. Now my son is in good health, and his finger movement has come back.
Posted On